
By now, you’ve likely heard of monkeypox, a rare disease caused by the monkeypox virus. Part of the same family of viruses as the variola virus, which causes smallpox, the monkeypox virus (MPV) most often causes a rash or lesions. Although experts have been aware of monkeypox for decades, this is the first global outbreak of the disease.
Prior to 2022, it has been known to primarily affect non-human primates and rodents in several western African countries. Some humans have contracted monkeypox by coming in direct contact with these infected animals. But the number of global cases we’re seeing now far surpasses the amount of past infections. As of August 22, 2022, the Centers of Disease Control and Prevention (CDC) reports 41,358 cases across 94 countries.
Several cities across the United States, including New York City and San Francisco, have either declared states of emergency in order to direct funds toward protecting folks from MPV or have at least cited it as a growing, imminent threat. So far, there have been 14,594 reported cases of monkeypox across the 48 contiguous states in the U.S. (via CDC, August 12, 2022).
While this global outbreak can affect anyone, the spotlight has been centered on the LGBTQ+ community, and, in particular, queer men and, to a somewhat lesser extent, sex workers. Although monkeypox is NOT a sexually transmitted infection (STI), sex often involves close contact, causing even more confusion around how the virus spreads.
This all makes for a complicated public health discussion: while everyone is susceptible to MPV, it is disproportionately impacting members of the LGBTQ+ community as well as sex workers. To protect everyone, especially those who are most vulnerable, it’s essential to untangle healthcare from both stigma and misinformation. So, here’s everything you need to know about monkeypox.
What Is Monkeypox Exactly?
Monkeypox is a disease caused by infection with the monkeypox virus. Even though it’s making headlines now, this virus isn’t anything new. The first reported case of monkeypox occurred in 1958 when it was discovered in monkeys being held in a lab in Copenhagen, Denmark.

Twelve years later, the first-known case of the virus in humans impacted six unvaccinated children. The first of those children to contract the virus was just 9 months old. By 1980, just a decade after these MPV cases, smallpox was considered eradicated. How does this relate to monkeypox?
Well, since the monkeypox virus is part of the same family as the virus that causes smallpox, worries surrounding it waned. The last naturally contracted case of MPV was reported in 1977, after all. Now, 45 years later, the first global outbreak of monkeypox is causing justifiable concern.
Reportedly, monkeypox will soon be given a new name, as suggested by 29 biologists at the World Health Organization (WHO) who found its current name discriminatory and inaccurate. But the stigma surrounding monkeypox extends further than its controversial name.
What Are the Symptoms of Monkeypox?
If you think you’ve been exposed to MPV, pay close attention to any potential symptoms. Often, the virus first causes a general discomfort, not unlike the symptoms of a common cold. These early symptoms can include swollen lymph nodes, general body aches and fever. After this initial round of symptoms, you’ll likely start to notice physical effects, too.

As you likely know, the most telltale symptom of the infection caused by MPV is a rash. At first, this reddish rash will look like pimple-like bumps, though lesions and scabbing can occur as the rash progresses. This rash can appear anywhere on the body — your face, arms, legs, hands, torso and genitals are all likely spots. Generally, the virus is self-healing, with the rash taking about two weeks to clear. Your symptoms may remain a bit longer, but, in most cases, go away on their own.
How Contagious Is Monkeypox?
The virus can be transmitted both by direct and close contact. Given this, a majority of infections have come as a result of sexual encounters, which, by nature, often require intimate contact. In fact, as many as 95% of cases have been linked to transmission during partnered sex.
However, it is important to remember that monkeypox is NOT an STI. Any form of sustained physical contact can spread MPV, and a person is considered contagious from the initial start of their symptoms until their rash has healed. This whole period can last anywhere from two to four weeks.
Monkeypox Is NOT an STI — So How Is Monkeypox Transmitted?
MPV is usually spread through a sustained amount of direct physical contact, but, as mentioned, it should not be mistaken as an STI. It’s not the act of sex that increases exposure, but direct bodily contact with an infected person. While experts aren’t suggesting people refrain completely from physical contact, it’s clear that sustained, direct contact is not advised, though there are precautions you can take.
Is Monkeypox Deadly — and How Is It Treated?
MPV is rarely fatal but the virus can be deadly. There have only been five recorded deaths worldwide at the time of writing. In general, monkeypox is considered a milder version of smallpox. As far as treatment goes, the CDC recommends Tecovirimat, an antiviral that can be administered either intravenously or orally.
The Monkeypox Vaccine: Why Isn’t It Accessible?
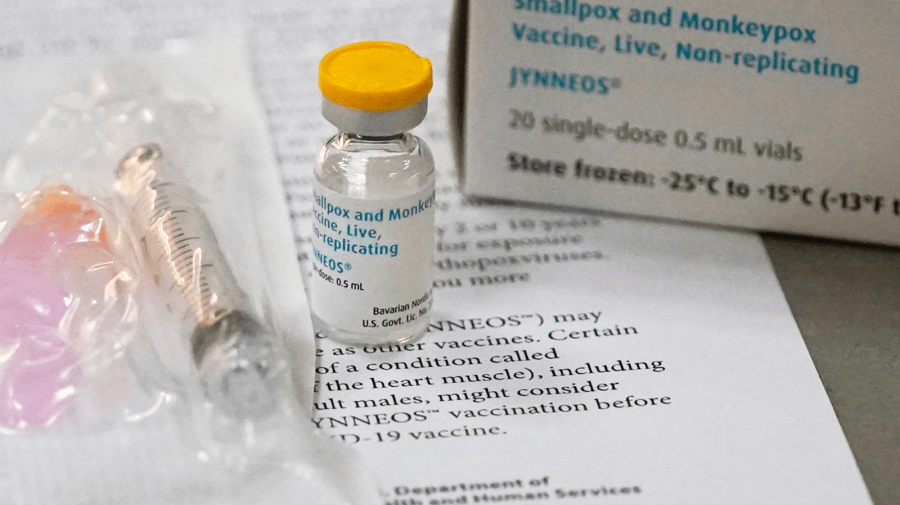
Currently, the U.S. Food & Drug Administration (FDA) has given the greenlight to two vaccines used to prevent monkeypox. These FDA-approved vaccines are referred to as JYNNEOS and ACAM2000. The unfortunate truth? The monkeypox vaccine is in limited supply. That said, health experts are aiming to first vaccinate those with a higher risk of being exposed to and/or contracting the virus and subsequent infection.
One of the vaccines, ACAM2000, can only be used in those without contraindicating conditions, such as a compromised immune system or a skin rash. As for JYNNEOS, the vaccine isn’t readily available because quantities of it are low worldwide. To put it bluntly, the U.S. is experiencing an MPV vaccine shortage while cases and exposure rates rise.
How Do We Protect LGBTQ+ People While Avoiding Stigma?
A group of researchers studied cases transmitted between April 27th and June 24th, 2022, and found that 95% of confirmed cases of the virus were transmitted during sex between men. But the language surrounding this public health crisis, and how it impacts men who have sex with men (MSM), is tricky, to say the least. There’s an understandable hesitation when it comes to focusing on MSM in the messaging surrounding monkeypox as it could worsen rampant anti-LGBTQ+ discrimination, or even cause folks to put out off seeking health services.
Callen-Lorde, a New York-based community health center that serves queer and trans patients, has been a leading voice during the outbreak. Understandably, it can be difficult to speak to a vulnerable community about their health and safety without making them feel targeted. Not to mention, dispensing necessary public health information can inadvertently cause those with bigoted views — or a lack of knowledge — to reinforce harmful stereotypes about MSM and queer people at large.

“Have open conversations with sexual partners about your status, and theirs. Lead with empathy!” Callen-Lorde suggests when it comes to what we can all do to address the MPV stigma. “We are all going through a scary time, but we are in this together. Do not blame or shame anyone — including yourself.” Both Callen-Lorde and the CDC also have resources for those looking to engage in safer sex practices or attend social gatherings while MPV cases are on the rise.
After all, anyone can contract the virus and the monkeypox infection. It shouldn’t be solely associated with a single group of people, such as queer men or sex workers. The best way to protect more vulnerable communities is to take action by dispensing more comprehensive information, ensuring vaccine access and equity and more. The goal is not to single out anyone — it’s to provide care to those who need it, all while encouraging risk mitigation.
Why Has San Francisco Declared a State of Emergency for MPV?
As of August 19, 2022, there are 638 cases of monkeypox in San Francisco alone. On the whole, California has 2,660 reported cases. As case numbers rise, San Francisco officials have realized that the city is a hotspot, making up 30% of reported cases throughout the entire state. Gavin Newsom, the governor of California, issued a state of emergency due to the spontaneous outbreaks of MPV.
While a state of emergency sounds dire, it’s not meant to incite panic. Instead, it allows officials to allocate more resources and direct more funding to the situation at hand. The San Francisco Department of Public Health (SF DPH) reiterates this stance.

“On July 28, 2022, the San Francisco Public Health Director issued a local public health emergency for monkeypox to harness resources, including efforts to obtain additional vaccine supply,” the department’s official website states. “This will also allow SF DPH and other health providers to prepare for an increase in cases and direct resources to testing, treatment, vaccination and community awareness.”
While San Francisco officials are making every effort to limit exposure and transmission, it’s clear that more vaccine shipments are needed to truly control the spread of monkeypox.
But San Francisco and other major cities like New York aren’t the only places on high alert. In a larger sense, the federal officials are taking note. Currently, there are over 14,000 reported cases of monkeypox in the U.S. Worldwide, the more than 40,000 confirmed cases of monkeypox are raising alarm bells, too. That said, with growing case rates and not enough vaccines to go around, it’s more important than ever to spread awareness about the monkeypox outbreak.






